Mechanisms involved in the control of central and peripheral inflammatory response in the experimental model of epilepsy with bone marrow stem cell transplantation
Research Coordinator: Jaderson Costa da Costa, MD, PhD < / p>
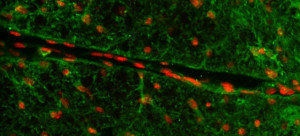
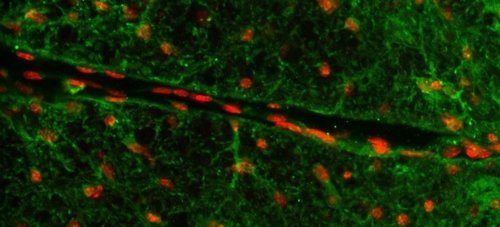
Summary of the work: Epilepsy is a brain disorder characterized by spontaneous and recurrent attacks of intense, synchronized and rhythmic triggering of neuronal populations. Pronounced inflammatory process has been described in the epileptogenic brain tissue of drug-resistant patients. In addition, changes in the blood-brain barrier and increased expression of pro-inflammatory cytokines highlight the activation of the inflammatory response during epileptogenesis. On the other hand, experimental strategies to block inflammation in the brain reduce the duration and frequency of attacks. Bone marrow stem cells (CTMO) have therapeutic potential in epilepsy. However, no previous study has been carried out on the possible anti-inflammatory action after the acute phase of epilepsy. The present work investigates the mechanisms involved in controlling the central and peripheral inflammatory response of epilepsy with CTMO transplantation.
Brain activation and recruitment of mononuclear cells have been implicated in the progression of epilepsy, but the role of specific populations and cytokines during development remains to be elucidated. For this, there is a proposal to investigate the IL-23 / IL-17 axis described as the final route for the recruitment of infiltrated cells to the brain. Then, it will be identified which population of infiltrates is being secreted IL-23, a modulator of Th17 cells. Subsequently, IL-23 and IL-17 with interfering RNA will be deleted to describe the functionality of the pathway in promoting inflammation. In addition, the presence of cells from the peripheral immune system may be linked to the cells or to chemical signals that are possibly released from the spleen. In this context, the objective is to investigate the role of the spleen in promoting brain inflammation and modulating CTMO. Taken together, these results propose to describe how CTMOs modulate inflammation through the IL-23 / IL-17 axis, decreasing parameters that lead to spontaneous and recurrent crises.
Research areas involved: Laboratory Neurosciences, Cell Signaling, Cell Therapy, Cell and Molecular Biology Laboratory - IPB.
Funding entity: Researcher from Rio Grande do Sul / FAPERGS