Doctoral student publishes article in international journal
Article by Ana Paula Bornes da Silva accepted in presitious journal Frontiers in Cellular Neuroscience
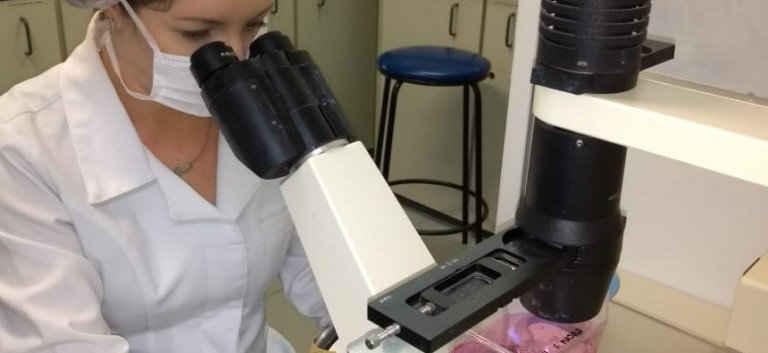
The doctoral student at PUCRS’ School of Medicine Ana Paula Bornes da Silva submitted the article entitled “The role of glutamatergic excitotoxicity neuromyelitis optica spectrum disorder”. The researcher works at the Laboratory of Cellular and Molecular Biology of the Brain Institute of RS, under the supervision of neurologist Dr Douglas Sato, Superintendent for Teaching, Research, Development and Innovation.
About the article
Authors: Ana Paula Bornes da Silva, Débora Guerini Souza, Diogo Onofre Souza, Denise Cantarelli Machado and Douglas Kazutoshi Sato.
In this review, the author describes how neurotransmitter (glutamate) alteration may have a negative role in Neuromyelitis Optica. This is an inflammatory autoimmune disease of the central nervous system (CNS) characterized by the production of autoantibodies against astrocyte aquaporin-4 protein.
In this article, she postulated that astrocytes are the key cells in glutamate metabolism imbalance and that this phenomenon occurs due to the action of autoantibodies produced in the disease. In this sense, the role of astrocytes in brain function and the importance of these cells in controlling CNS glutamate levels have been described.
The article suggests that glutamate uptake by astrocytes is reduced in neuromyelitis. This would be attributed to the partial loss of activity of the type 2 glutamate transporter known as EAAT2 present in these cells. In addition, the author suggested consolidated pharmacological strategies already to the treatment of other CNS diseases, as an additional treatment for neuromyelitis optica.
Glutamate is a neurotransmitter that, when found in high concentrations in the brain, eventually interferes with the functioning of nerve cells, killing neurons and other healthy cells. The student hopes to have a better understanding of the mechanisms of the disease. In the future, she also wants to propose therapies to reduce the toxicity of glutamate to keep neuromyelitis lesions from growing. ”, Ana Paula Bornes da Silva says.
About the disease
Neuromyelitis optica is a demyelinating disease. Damage in the myelin sheath keeps the nerves from conducting nerve impulses properly. Sometimes nerve fibers are also affected. If the myelin sheath is able to repair and regenerate on its own, nerve function is completely restored. However, when the myelin sheath is severely injured, the underlying nerve fibers may die. The nerve fibers of the central nervous system (brain and spinal cord) cannot fully self-regenerate. Therefore, these nerve cells are permanently injured.
The symptoms are somewhat similar to those of multiple sclerosis, except that in neuromyelitis optica, only affects the eyes and spinal cord get affected. On te other hand, multiple sclerosis also affects the brain. Neuromyelitis optica causes inflammation of the optic nerve. It may affect one or both eyes. It is characterized by episodes of eye pain, blurred vision and in severe cases leads to vision loss.
Days or weeks later (sometimes even years), members are affected. People may temporarily lose sensitivity. They may have intense muscle spasms and their arms and legs may become weak and sometimes paralyzed. They may also be unable to control bladder and bowel functions.
In some people, the part of the spinal cord that controls breathing becomes inflamed, leading to life-threatening breathing.
The disease progresses differently in each person. As the disease develops, people may experience painful, frequent and brief muscle spasms. Finally, blindness, loss of sensation and muscle weakness in the limbs, and bladder and bowel dysfunction may be permanent.
Nuromyelitis optica is a demyelinating disease. It occurs when the body’s immune system is not working properly and attacks the body’s own tissues. In neuromyelitis optica, the target of autoimmune attack is a protein called aquaporin-4, which is present on the surface of the supporting cells (called astrocytes) in the brain, spinal cord and optic nerves. Binding of autoantibodies against aquaporin-4 triggers multiple cell and brain tissue damage, leading to secondary demyelinating condition.