Coronavirus: The long list of possible sequels to Covid-19
Photo: Lucy NicholsonI / Reuters
BBC article interviews InsCer director Jaderson Costa da Costa about the possible impacts of Covid-19 on the human brain. Check it out in full:
Seven months after the emergence of covid-19, more than 18 million have already been infected with the new coronavirus in the world and about 11 million patients are considered recovered.
On the one hand, the scientific community is still looking for a vaccine against Sars-CoV-2. On the other hand, doctors try to understand what medium and long-term consequences the virus can bring to those who have already come into contact with it.
A series of studies released in recent months and the clinical observation of professionals on the front line indicate the possible sequelae that the disease can leave - although it is not possible to say whether they are temporary or permanent.
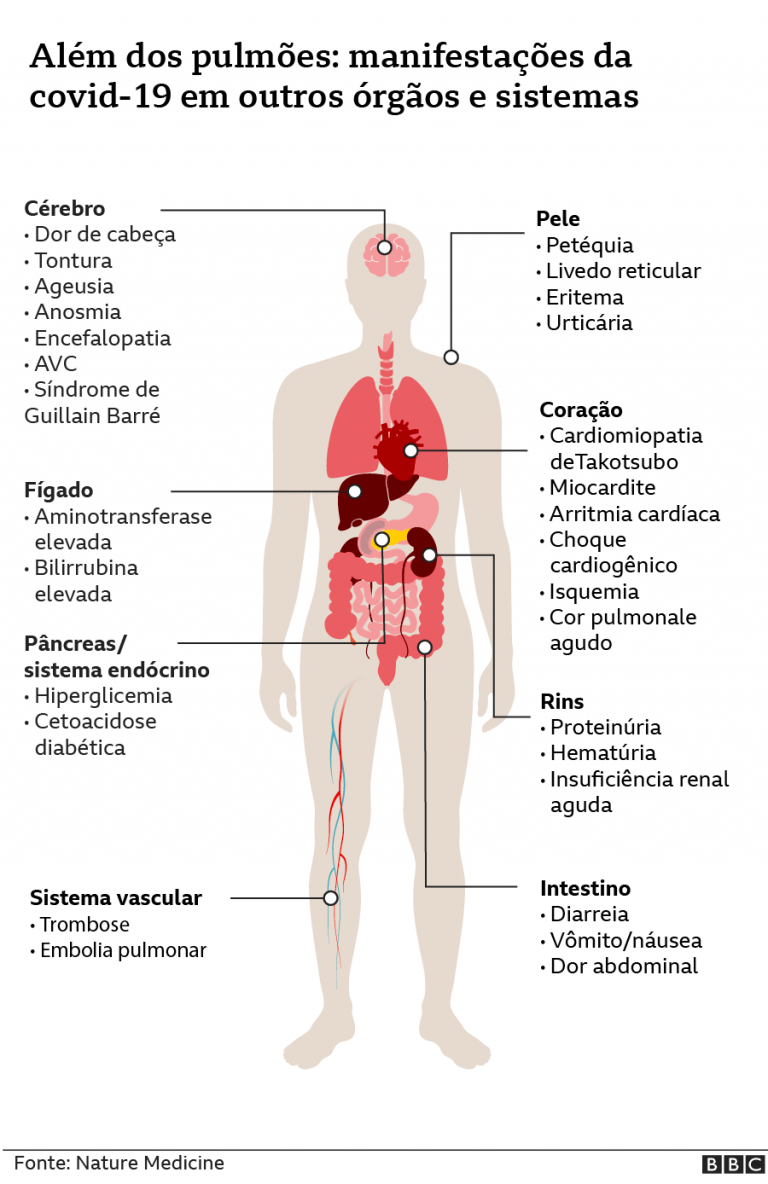
It is already known, for example, that some symptoms can persist not only among those who have had more severe cases of the disease and that, in addition to lung damage, Sars-CoV-2 can affect the heart, kidneys, intestine, the vascular system and even the brain.
Breath compromised after discharge
The pulmonologist Gustavo Prado, from the German hospital Oswaldo Cruz, says that he has received a significant volume of patients who had moderate covid-19 and report, for example, tiredness and shortness of breath.
One of the first studies on the lung function of patients who had just been discharged in China indicated, in April, that the reduction in lung capacity was one of the main consequences observed even among those who did not become critical.
Published in April in the European Respiratory Journal, the work highlighted the occurrence of similar phenomena in epidemics caused by other coronaviruses, those of Sars and Mers, in which the sequelae lasted for months or years in some cases.
More recently, a study published in the Journal of the American Medical Association (JAMA) found that, among 143 patients evaluated in Italy, only 12.6% had been admitted to an ICU, but 87.4% reported persistence of at least one symptom, including fatigue and shortness of breath, more than two months after they were discharged.
“We have even seen a latency for the full recovery of patients who have had moderate conditions”, says the pulmonologist at Fleury João Salge.
Many of these patients, he says, return to day-to-day activities, but report tiredness and see their productivity and quality of life affected.
To them, the doctor has recommended that they do physical exercises, respecting the limitations of the moment, and that they try little by little to challenge the organism to recover their conditioning.
But it is not yet known how long these symptoms can last.
Pulmonary fibrosis
In the most severe cases, it is possible that there are permanent sequelae, such as pulmonary fibrosis, a chronic disease characterized by the formation of scars in the lung tissue.
"The scar fills the space, but it does not have the same elasticity, the same characteristics as the original tissue", explains Prado.
Thus, the lung expands less, or with greater difficulty, with a consequent loss of efficiency in gas exchange. With reduced respiratory capacity comes frequent shortness of breath and tiredness.
Fibrosis can be caused by the intense and widespread inflammation that the body causes to try to expel the virus from the body. In this case, it is a consequence of the natural repair process of the damaged tissue.
But it can also be the result of the treatment itself, when the patient is intubated, for example.
“Although necessary in severe respiratory syndrome, inadequate ventilation can impose stress on lung tissues - due to exaggerated distention, the maintenance of high pressures in the filling of the lungs or the excessive supply of oxygen”, exemplifies Prado.
It is the so-called ventilation-induced lung injury, or VILI (acronym of the English expression “ ventilator-induced lung injury “), which can develop into fibrosis.
Post-ICU syndrome
Far from being exclusive to covid-19, this type of injury characterizes several more severe respiratory syndromes.
The particularity in this case is the fact that the hospitalization interval for patients infected with the new coronavirus is usually longer, which increases the likelihood of this type of sequel.
“They stay intubated for a long time, tracheostomized, in ECMO (acronym for“ extracorporeal membrane oxygenation “, or oxygenation by extracorporeal membrane, which consists of using a machine that performs the function of the heart and lungs and pumps blood), ”says pulmonologist and Fiocruz researcher Margareth Dalcolmo.
The prolonged period in the hospital also increases the chances of another problem that affects those affected by serious infections: the post-ICU syndrome.
Symptoms range from loss of muscle strength, changes in sensitivity and motor strength due to nerve dysfunction to depression, anxiety, cognitive changes, impaired memory and reasoning ability.
Severe cases of covid-19 are in the minority, about 5% of the total. In the face of a major pandemic, however, a small percentage can mean high absolute numbers. Among about 11 million recovered, for example, the 5% become 550 thousand.
In this sense, Prado, from Hospital Alemão Oswaldo Cruz, draws attention to the fact that part of this large contingent will need medical monitoring for some time, either in SUS or in private health.
“And most of the patients still belong to the economically active population. We need to demystify this idea that it is only the elderly with comorbidity ”, he adds.
‘Ground zero’
The lungs are a kind of "ground zero" for Sars-CoV-2. Once the virus manages to cross our immune barrier and installs itself in the lung, it continues to damage other organs.
An article published in April in the journal Science highlighted that a possible signal for the most vulnerable regions of the body would be those rich in receptors called ECA2 (angiotensin-converting enzyme 2).
With the function of regulating blood pressure, these proteins stay on the cell surface and are used as a gateway by the virus, which uses the cellular structure to reproduce.
In addition to the lungs (more specifically the pulmonary alveoli), ECA2 is also found in organs such as the heart, intestine and kidneys - which have suffered major injuries in patients in a more serious condition.
“That is why we say that covid-19 is a systemic disease, and not just a respiratory one”, says Dalcolmo, from Fiocruz.
Scientists are still investigating whether this damage is caused directly by the virus or by indirect factors linked to the disease.
One possibility, for example, is that the “inflammatory storm” that the immune system generates to try to fight the virus, flooding the body with cytokines, ends up damaging these organs. Part can also be a consequence of the infection itself.
Kidneys and heart
Regardless of the cause, scientists seek to understand which of these effects have short, medium or long term consequences.
A recent study - with worrying results - conducted in Germany pointed out that, among 100 recovered patients, 78% had some kind of anomaly in the heart more than two months after discharge. Much (67%) had had a mild form of the disease and had not even been hospitalized.
In the case of kidneys, the evidence shows a high incidence of bankruptcy among the most serious cases of covid-19.
Brain
The occurrence of a series of neurological symptoms ranging from mental confusion and cognitive impairment to delirium has also been documented among patients with covid-19.
In Brazil, a task force from the Rio Grande do Sul Brain Institute (Inscer), linked to PUC-RS, investigates, among other fronts, what sequelae may be caused by these symptoms.
The neurologist Jaderson Costa da Costa , who coordinates the group, says that, among the most serious cases treated by the team at Hospital São Lucas, in Porto Alegre, seizures, cases of syndrome Guillain-Barré (which attacks the nervous system and causes muscle weakness) and encephalitis, the inflammation of the brain parenchyma.
An a recent study from University College London drew attention to a rare and severe case of encephalitis that has affected some patients with covid - the disseminated acute encephalomyelitis.
Vascular system
Another neurological complication that doctors have observed in patients with severe cases is the occurrence of strokes.
For some reason that scientists are still unaware of, Sars-CoV-2 increases the tendency of blood to clot.
So much so that a protein fragment used in the diagnosis of thrombosis, the D-dimer, became a marker of severity for patients with covid.
"When he is high, it is a sign of possible evolution to a more serious condition", says the pulmonologist of Fleury João Salge.
Unrestrained coagulation can lead to venous thromboembolism - blockage of a blood pathway, which can end up causing stroke, pulmonary embolism or extremity necrosis, leading to the need for amputation, which has also been seen in patients with covid .
“This dichotomy between‘ died ’and‘ survived ’is wrong,” says pulmonologist Gustavo Prado, calling attention to the need to discuss rehabilitation of recovered people.
For him, the wide range of possible consequences left by covid-19 and the size of the affected population should transform this recovery process into a broader issue, involving a public health and social assistance strategy and including health professionals from different fronts.